Lupus anticoagulant testing aids in the diagnosis of autoimmune blood clotting disorders.
ARUP Laboratories now offers an updated lupus anticoagulant reflexive panel that can detect and neutralize several commonly prescribed anticoagulant medications and limit their impact on test results. By neutralizing possible interfering medications, the assay reduces the likelihood of false-negative and false-positive results.
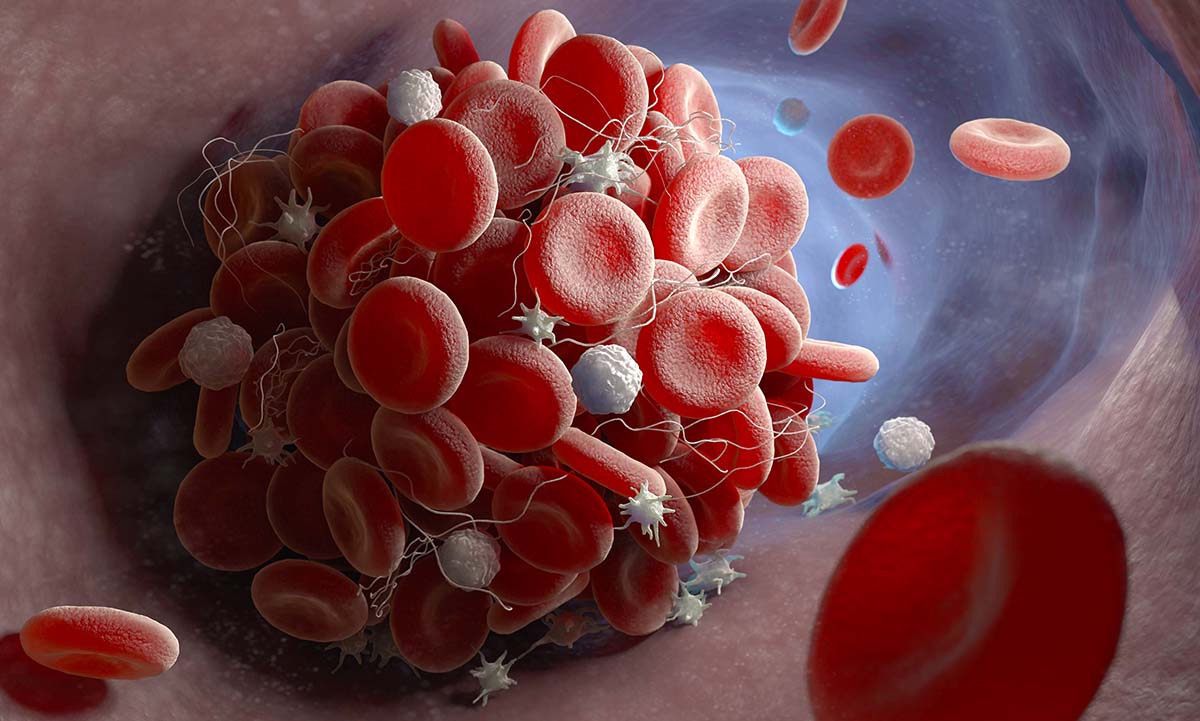
Detecting lupus anticoagulant antibodies can aid in the diagnosis of antiphospholipid syndrome (APS), a rare autoimmune disorder in which autoantibodies directed against proteins bound to phospholipids result in thromboses.
“This test has the potential to have a major impact on a patient’s treatment,” said Kristi Smock, MD, chief medical director of Research and Development and medical director of the Hemostasis/Thrombosis Laboratory at ARUP. “It can help determine if patients need long-term anticoagulation to prevent blood clots. However, anticoagulation can have associated bleeding risks and should only be used when appropriate.”
Smock and her colleague, Karen Moser, MD, medical director of the Hematopathology and Hemostasis/Thrombosis Laboratory, collaborated on the development of the assay.
“We [Karen and I] both exhaustively researched the literature, including different guidelines and different pieces of evidence, to put together the best, most modern version of this test,” Smock said.
Lupus anticoagulant testing uses multiple clot-based assays to detect the presence of antibodies that increase the risk for blood clots. These clot-based assays are prone to interferences from anticoagulants, making diagnosis more challenging in patients taking anticoagulant medication.
“There are a number of different expert consensus guidelines related to this type of testing, but they all uniformly caution against testing patients who are anticoagulated,” Smock said.
However, it’s commonplace to receive samples from patients who are on anticoagulant medication, according to Smock and Moser, who wanted to pursue a more robust reflexive testing strategy that could better address the interferences that arise in routine clinical practice.
Not only has the assay been updated to neutralize drug interferences, but the reports of its results have been updated to provide quantitative results. This will increase transparency in reporting and better aid clinicians making decisions in clinical contexts.
Medical directors and fellows are available to consult with clinicians regarding test result interpretation through ARUP’s Path-On-Call service.
“This panel is robust and high quality, and it has been carefully vetted,” Moser said.
Kellie Carrigan, kellie.carrigan@aruplab.com