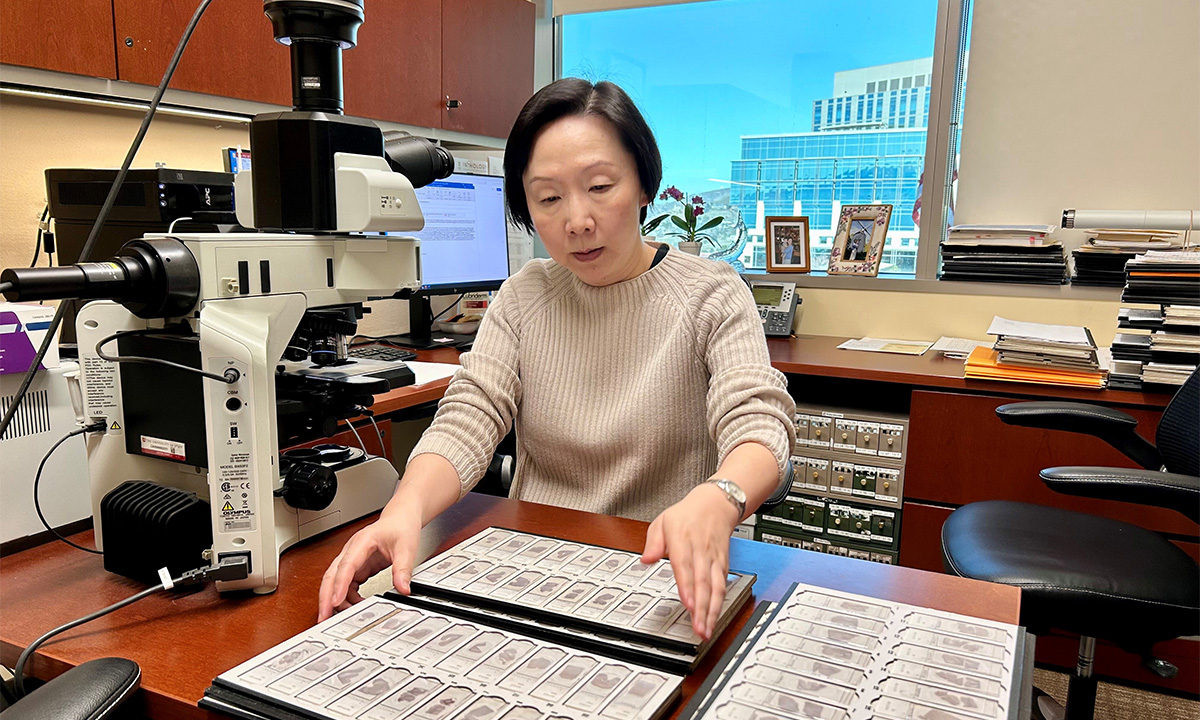
An expert in TAR DNA-binding protein of 43 kDa (TDP-43), neuropathologist Qinwen Mao, MD, PhD, subspecialty director of Neuropathology at ARUP, is working to identify biomarkers that predict the presence of TDP-43 pathology to contribute to the diagnosis of frontotemporal lobar degeneration (FTLD) and Alzheimer’s disease.
As a scientific manager in Research and Development (R&D) at ARUP Laboratories, Sonia La’ulu helps validate tests that provide answers in the clinical diagnosis of disease. It’s rewarding work—a calling that she finds particularly meaningful when it touches close to home.
A test that ARUP will offer for the first time starting in May has La’ulu particularly excited. Alzheimer’s Disease Markers, CSF, will be ARUP’s new test for biological markers (biomarkers) of Alzheimer’s disease (AD). More biomarker tests are in the development pipeline now that the FDA has approved the first AD therapies and testing is needed to help identify candidates for treatment and monitor their response to therapy.
For La’ulu, the potential for earlier diagnosis and treatment of the disease that afflicted her paternal grandmother means that she and other family members who witnessed their matriarch’s decline can rest a little easier as they age.
“To have an FDA-approved test, as well as FDA-approved therapies, has created a feeling of hope, and that’s huge,” she said. “It’s just huge.”
Growing Need for Earlier Testing
The Alzheimer’s Association estimates that 6.7 million Americans age 65 years and older are living with AD. As the U.S. population ages, incidence of the disease will only increase, the association says, making improved diagnosis and treatment imperative.

Recognizing an opportunity to meet the growing need for tests, ARUP has prioritized innovation in diagnostics for AD and other neurodegenerative diseases, said Robert Ohgami, MD, PhD, FCAP, vice president of the ARUP Institute for Research and Innovation in Diagnostic and Precision Medicine™ (R&I Institute). As ARUP prepares to launch the new AD biomarker test on cerebral spinal fluid (CSF), ARUP researchers have begun collaborating with industry partners in the exploration of both plasma biomarker immunoassays and mass spectrometry tests, he said.
Ohgami views the collaborations as ideal projects for the R&I Institute, which ARUP formed in July 2023 to hasten development of novel tests. “ARUP has broad expertise in translating innovation to application, and we continue to seek out partners with whom we can work to develop diagnostics that will have clinical impact,” he said.
ARUP’s New Biomarker Test
AD traditionally has been diagnosed using cognitive tests and structural imaging such as magnetic resonance imaging (MRI) or computed tomography (CT) scans to detect damage that has already occurred in the brain. Newer tests, though, including ARUP’s new test, seek to evaluate biomarkers that signal the presence of disease in its early stages, when it may be possible to slow its progression. In the case of AD, relevant biomarkers include beta amyloid and tau proteins.
As we age, nerve cells in our brains start to break down, in part due to the development of plaques (aggregates of beta amyloid protein fragments) that build up between nerve cells, and tangles, or twisted fibers of tau proteins that accumulate inside cells, according to the Alzheimer’s Association. Most people develop plaques and tangles in the brain with age, but researchers have shown that those who develop AD have more plaques and tangles, and they develop them in predictable patterns.
Imaging technologies, such as positron emission tomography (PET) scans, aid in the diagnosis of AD because they can detect amyloid plaques and disruption of normal brain function, said Kelly Doyle, PhD, DABCC, FAACC, medical director of Special Chemistry and Endocrinology at ARUP. PET scans, though, are costly, and their availability is limited, so clinicians welcome tests such as ARUP’s new AD biomarker test on CSF to help diagnose AD.

The new test uses an FDA-approved kit and instrumentation manufactured by Roche. Its performance is backed by significant data, and test results have been demonstrated to closely correlate with amyloid PET scan results, Doyle said. Current National Institute on Aging/Alzheimer’s Association guidelines specify that biomarker-based AD diagnosis can be established only via PET scan or by measuring biomarker concentrations in CSF.
The soon-to-be-available ARUP test (No. 3017653) is intended for use in patients older than 55 years. It measures total tau, beta amyloid 1-42 (Aβ 42), and phosphorylated tau 181 (p-tau 181) concentrations in CSF to produce two ratios: total tau to Aβ 42, and p-tau 181 to Aβ 42, said Heather Nelson, PhD, DABCC, ARUP medical director of Clinical Chemistry. Interpretation of the ratios does not establish a diagnosis of AD or other cognitive disorders, but it can contribute to an AD diagnosis when considered along with other clinical evaluations.
She said that individual concentrations of the biomarkers are not reported “because the ratios are more sensitive and specific for the disease than looking at any of the individual biomarkers.” In addition, she and Doyle believe more research and clinical data are needed before conclusions can be drawn as to whether specific individual values are indicative of AD.
Also, if ARUP were to report individual biomarker concentrations, its CSF biomarker test would no longer be FDA approved, Nelson said. Rather, it would be considered a laboratory-developed test.

“We decided to stick with the on-label test, at least for now,” Doyle said.
He and Nelson believe the launch of the CSF test will pave the way for ARUP to bring on a plasma biomarker test as a next step. Exploration of several options for a test on plasma, most of which are focused on detection of phosphorylated tau 217 (p-tau 217), are underway.
“The promise is there, and there’s obviously an allure to having a test for which you don’t have to do a spinal tap,” Doyle said.
Research Into Other Biomarkers
Still preliminary, but equally exciting, is neurodegenerative disease biomarker research underway in the University of Utah laboratory of neuropathologist Qinwen Mao, MD, PhD, who is also subspecialty director of Neuropathology at ARUP. Her research centers on TAR DNA-binding protein of 43 kDa (TDP-43) and its relevance in frontotemporal lobar degeneration (FTLD), as well as in AD.
Already, Mao’s research has shed light on TDP-43 species and their markers, as well as on how they are associated with neurodegeneration. She is working to explain how TDP-43 conformational changes and accumulation cause neurodegenerative symptoms that can vary broadly, from behavioral dysfunction to language dysfunction to progressive aphasia.
Mao said her goal is to identify biomarkers that predict the presence of TDP-43 pathology to contribute to the diagnosis of FTLD and AD. Working with Lisa Peterson, PhD, D(ABMLI), ARUP medical director of Immunology, and others, she ultimately aims to develop a plasma immunoassay for TDP-43 markers.
“To develop treatments for diseases, we must understand what causes them at the molecular level. That is why this work is so important,” Mao said. “Our hope is that we will one day be able to identify and treat the exact cause of FTLD and other disorders.”
More to Learn About Diagnosis, Treatment
Even though the promise of improved diagnosis and treatment for AD and other neurodegenerative diseases has never been greater, researchers urge caution as discovery and development continue.
As more tests become available, Doyle said, he and other clinical chemists advocate for their use in clinical settings by providers with expertise.
“Whatever result you’re going to get and provide to a patient, it needs to be mediated through a clinician who knows how to handle these cases specifically,” he said. “You wouldn’t want to hand a result to someone that says they either have signs of AD or are at risk for AD without them knowing what the next steps are, and especially when these therapies may not be available or insurers may not pay for them.”
Amid the intense interest and infusion of resources to fight neurodegenerative disease, clinical expertise will certainly grow, as will consumer knowledge and understanding of options.
La’ulu will be following every development closely.
“I’m hardly alone. So many people know and care about someone affected by these diseases,” she said. “We have much to learn, but we also have every reason to hope.”
Lisa Carricaburu, lisa.carricaburu@aruplab.com
















