Four different algorithms to lead clinicians through the correct approach to thyroid testing are available on arupconsult.com.
Thyroid disease is common and affects about 20 million Americans, most of them women. According to the American Thyroid Association, women are five to eight times more likely than men to have thyroid problems, and 60% of people with thyroid deficiencies are unaware of their condition. Undiagnosed thyroid disease may put patients at risk for serious conditions, such as cardiovascular diseases, osteoporosis, and infertility. January is Thyroid Disease Awareness Month, and ARUP Laboratories offers evidence-based and comprehensive thyroid disease testing resources on ARUP Consult. ARUP’s medical directors and faculty members at the University of Utah School of Medicine contribute to and review the ARUP Consult topics.
One reason thyroid disease is underdiagnosed is that the associated symptoms are nondescript: fatigue, unexplained weight changes, sensitivity to heat and cold, depression, irritability, constipation, diarrhea, dry skin, hair loss, fast heart rates—and the list goes on, depending on the cause of the disease.
Thyroid conditions stem from either hypothyroidism, an underactive thyroid, or hyperthyroidism, an overactive thyroid. Both conditions can manifest with some of the symptoms listed above. Because the clinical signs are nonspecific, laboratory testing is required for diagnosis, and accurate diagnosis is necessary for appropriate treatment, but testing is complex.
First, it can be difficult to determine appropriate reference intervals for the interpretation of thyroid function tests.
“Reference intervals for thyroid function tests should be population specific, because so-called ‘normal’ values depend on age, sex, and other variables,” said Joely Straseski, PhD, MS, MT(ASCP), DABCC, ARUP section chief of Chemistry and medical director of Endocrinology.
Another major challenge is assay interference. There are many medications that affect thyroid function testing, including estrogens, such as those found in birth control pills. Biotin, a common over-the-counter supplement, can cause the results of several thyroid function tests to appear abnormal, when they are in fact normal. Additional information about biotin interference with thyroid function and other tests is available on ARUP’s Biotin Interference page.
Other causes of interference, including macro thyroid-stimulating hormone (macro-TSH), antistreptavidin antibodies, antiruthenium antibodies, thyroid hormone autoantibodies, and heterophilic antibodies, are discussed in the ARUP Consult Analytical Considerations in the Evaluation of Thyroid Function topic.
Thyroid disease testing is especially important in pregnancy because maternal hypothyroidism and hyperthyroidism can have serious adverse consequences. However, the thyroid gland undergoes changes that complicate testing during pregnancy, which results in possible increases in the concentrations of thyroxine-binding globulin, total T3, total T4, and serum thyroglobulin, as well as decreases in thyroid-stimulating hormone (TSH) and serum free T4 concentrations.
“All of these may change as pregnancy progresses, and reference intervals should be adjusted accordingly,” Straseski said. The ARUP Consult Thyroid Disease in Pregnancy topic details recommendations for pregnancy-specific reference intervals to ensure appropriate treatment and management of thyroid disease during this critical period.
ARUP’s thyroid disease testing resources were designed to help clinicians quickly access up-to-date information and order the right tests. They are organized into eight different topics, including:
- Initial Evaluation of Thyroid Function
- Analytical Considerations in the Evaluation of Thyroid Function
- Hypothyroidism
- Thyrotoxicosis
- Thyroid Disease in Pregnancy
- Autoimmune Thyroiditis
- Thyroid Nodules
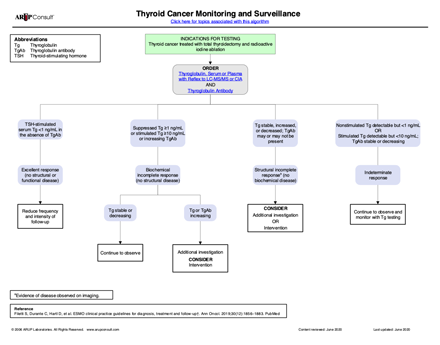
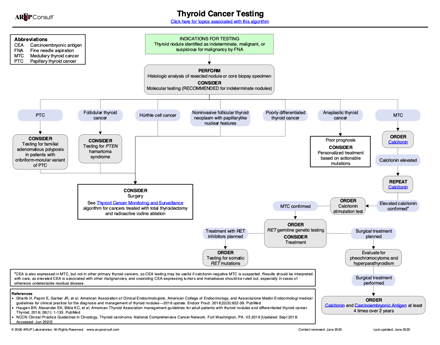
- Thyroid Cancer
Algorithms like the ones above are also available to lead clinicians through testing based on the clinical context and findings.
“We are distilling down what can be really complicated information and making it accessible and delivering it in a useful way so clinicians can find all the answers they need,” Straseski said.
The complete thyroid disease resources are available at arupconsult.com. They feature information from clinical associations, public health agencies, and ARUP experts, including Straseski; Kayode Balogun, PhD, a former clinical chemistry pathology fellow at the University of Utah School of Medicine; and Benjamin Kukull, MD, a former molecular genetic pathology fellow at the University of Utah School of Medicine. These reviewers contributed expertise and reviewed the resources.
Bonnie Stray, bonnie.stray@aruplab.com