A Real Page Turner
Extracting Vital Clues from the Stories within Our Genes
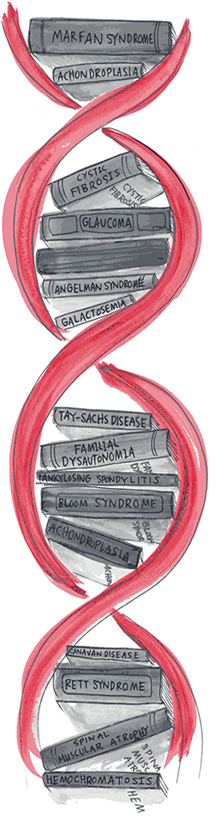
What if our bodies were libraries? And the thousands of books, instead of sitting on the shelves, were circulating through our bodies? Each book a gene; each gene, a story. Written into these stories are vital, personal clues for identifying and treating disease.
Delving into these discoveries requires sophisticated technology and the biocomputing prowess to go with it. Next-generation sequencing (NGS) is one such technology that breaks open stories, so sequence analysts and ARUP medical directors can begin looking for mutations or variants in a patient who may desperately need answers. NGS delves into the DNA found in the patient’s saliva, a cheek swab, blood or—more invasively—the DNA found in a tumor via biopsy or surgery.
Patients who receive NGS testing may have a suspected inherited disease (that could also involve testing their family members), or they could have cancer and need the improved information that NGS cancer testing can provide to better select and manage their chemotherapy.
“Once the sequences of DNA building blocks are deciphered from a patient’s DNA, highly developed and complex computerized analysis known as bioinformatics must next occur, to decipher the millions of data points and unravel whether genetic abnormalities are present in a patient’s sample, “explains Mary Bronner, MD, division chief of Anatomic and Molecular Oncologic Pathology at ARUP.
Finding the answers is no small task. Keeping with the book analogy, medical director Todd Kelley, MD, says,
“Imagine all the sentences from all these books [genes] are jumbled up. Now reconstruct them and put them back into the right place in each book.” Sequence analysists must then “read each book and look for potential errors.”
Todd Kelley, MD, Medical Director, Molecular Hematopathology and Hematopathology
These analysts look closely at these “errors” or aberrations, some of which may be typical gene variants (i.e., a variant determining your eye color). It is the variants that may express pathogenic or disease-causing changes—mutations in a gene—that they are most interested in further analyzing.
Increasingly, the use of NGS in laboratory testing is actively driving patient care. While NGS has a strong track record in research, ARUP has been using it to deliver NGS-based results to clinicians since 2012. Bioinformatics at ARUP spans five areas of clinical focus: molecular genetics, immunology, hematopathology, solid tumor pathology, and soon infectious diseases. Application of NGS technology to these areas has resulted in massively complex data needs.
“Bioinformatics is truly at the heart of the successful application of NGS technology in medicine,” says Frederick Strathmann, PhD, interim scientific director, Biocomputing and medical director, Toxicology. “ Without the bioinformatics aspect, the sequencing sits in limbo and cannot be fully appreciated. It is an integrated process that involves numerous technologies and highly skilled people to provide actionable information to physicians.”
NGS Testing: Pipeline from Patient to Diagnosis

Ashley
Ashley developed easy bruising and had frequent nose bleeds and infections over the last few weeks. An analysis of her blood revealed anemia and a low platelet count. Her doctor extracted some bone marrow to send to ARUP for analysis.

Charlie
Charlie passed out on the basketball court. Because he’s an avid athlete and only 17, this was surprising. His doctor ran some cardiology tests and then sent a blood sample to ARUP for analysis. The doctor suspected aortopathy, a disease that can cause the aorta (the heart’s main artery) to rupture. It can run in families or not.
Genomics Lab
In each lab, using NGS instrumentation, laboratory staff extract DNA from areas of interest and prep it for sequencing. This process replicates the DNA millions of times. Such amplification of the DNA allows scientists to home in on targeted areas and see DNA reactions happening simultaneously. In contrast, the Sangar method, an older technology, can only look at one specific area/ reaction at a time.
Bioinformatics Mining
Both labs send this NGS raw data to their team of bioinformatics experts. Remember the jumbledup sentences from millions of books? This is it.
Their job is to organize this raw data. Essentially the DNA is cut up into lots of little pieces then reassembled so it is sensible and can be interpreted more easily and accurately.
Sequence Analysis
Sequence analysts generate reports that contain changes, or variants, that are found in the patient’s DNA and information related to those variants. They begin by interpreting the data and comparing findings to gene-specific databases and medical literature.
They are looking for whether this variant has been reported previously. If so, is it connected to a disease? Or is it a variant found in a large segment of the population and therefore likely benign?
Medical Director Analysis
Nearly 30 of ARUP’s medical directors are involved in NGS testing and in this final stage of analysis, they are providing a secondary review and ensuring that all clinical aspects have been considered. This means providing clinicians with an accurate and comprehensive report of their patients’ results.
To further ensure accuracy, a medical director may pick out the variants of interest and send them in for Sanger evaluation to confirm their role in diagnosis. Sanger is an earlier method used in DNA sequencing and, while slower, it is still considered the gold standard, but that may change as NGS evolves.

Ashley
Ashley and her family learned that she had acute myeloid leukemia, a type of blood cancer. The NGS results helped her doctor determine that a bone marrow transplant would be her best chance for a long-term cure.

Charlie
Charlie and his family found out that he tested positive for a mutation that causes Marfan syndrome, a type of aortopathy. Based on this information, his doctor prescribed medication and discussed the lifestyle changes Charlie needed to make and the need for ongoing screenings throughout his life. Charlie also learned that his children would have a 50 percent risk of inheriting the disease

















 HOME
HOME