
It’s Not Easy Being a Hospital Laboratory
We Get It!
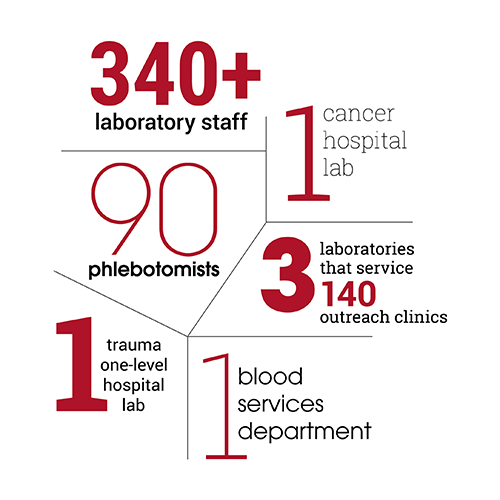
Hospital laboratories are a unique entity within the hospital. Often, they are hidden. Often, they’re the fall guy when something “test related” goes awry. Yet in-hospital laboratories are indispensable to patient care. As part of the University of Utah Health academic-medical system, ARUP runs labs in the U of U hospital and in the Huntsman Cancer Institute, and services 140+ outreach clinics (see infographic).
“We understand the challenges hospital laboratories face because we’ve faced them, too,” says Jason Goodfellow, information technology (IT) manager of U of U Hospital labs. “We feel their pain.”
Goodfellow draws on his own experience and expertise to consult with ARUP clients about hospital operations, IT, phlebotomy, process improvements, and specimen receiving. Issues that clients face related to Centers for Medicare and Medicaid Services (CMS) payments, overloaded emergency departments, communication, and space constraints are all similar to ARUP’s own experiences in running a hospital laboratory.
“We also understand the challenges of communicating with the hospital so they can better discern the issues that the laboratory faces,” says Jo D Fontenot, ARUP senior operations director for the U of U Hospital labs. She oversees phlebotomy and support services, client services, operations, clinical labs, and blood donor services. “We’ve had to learn how to advocate for the lab, solve problems, and collaborate in a system-wide approach, not in a vacuum.”
With more than 60 years of experience between them, both Fontenot and Goodfellow know that all too often when things go wrong, fingers get pointed at the lab. Here, they discuss the issues they’ve faced, solutions they’ve found, and the work that still needs to be done


How can a hospital lab avoid being a silo? What has ARUP done to overcome this?
JF—Become involved with hospital management. Reach out to nursing management and quality teams to collaborate on process-improvement opportunities. If the hospital has a patient safety committee, get involved. Committees like this are a great platform for others within the hospital to understand the challenges related to the hospital’s lab.
JG—We’ve found that IT needs to be significantly involved in the clinical decision support team and the electronic health record (EHR) operations team within our hospital. Many institutions operate with a centralized IT department and this makes individual IT solutions improbable. On the laboratory side, we embed IT analysts in each department, which allows us to customize IT services.
JF—We did all this, and then we developed a Laboratory Process Improvement (LPI) committee that includes representation from nursing services and informatics, hospital quality, emergency department staff, IT, Epic super users, and patient safety.
This committee has helped people realize that, in many scenarios, the lab isn’t really at fault, and that inefficiencies are a system-wide issue. For example, a provider may add a test to an order, but it is added incorrectly so the lab doesn’t receive the add-on. Or laboratorians may end up with a sample but no order, or have a sample with a collection date and time that don’t match the order. This is an interface issue between two different electronic systems, not solely a lab issue.
JG—As part of our LPI committee, IT representatives help address persistent process failures. We work with the hospital IT staff and quality teams to assess and fix issues. For example, if there is an inpatient location that has a high number of errors or complaints (e.g., incomplete labs, slow turnaround times), we’ll go work directly with their staff to figure out what we can do as a team to improve outcomes.
“We understand the challenges hospital laboratories face because we’ve faced them, too.”
Jason Goodfellow, ARUP
The lab also provides training to medical staff on phlebotomy procedures and point-of-care (POC) testing. Our two laboratory liaisons work directly with nursing and clinic personnel to address questions or concerns in person. This goes a long way in bridging the lab-versus-hospital gap.
JF—We also provide tours of the laboratory to current and new nursing personnel. Otherwise, it’s just a black box to them.
What are some observations or misperceptions you can share regarding hospital labs?
JF—There’s a real lack of appreciation regarding the complexity of laboratory testing and the preanalytic impact. Let’s say a laboratorian recognizes a sample is compromised based on how it was collected and requests a recollection. Nursing personnel can become frustrated with this delay because they don’t understand that the contamination may not be detected until the test is run.
Because hospital labs are often not visible, we forget that there are people who care deeply about the patient’s well-being. If lab staff recognizes a sample has been compromised, they’ll reorder it because they don’t want to risk inaccurate results that could affect the patient’s care.
There is also a lack of understanding of nurses’ and providers’ roles in the delivery of timely and accurate patient results. This includes accurately placing and releasing orders, correctly collecting and labeling the specimens, and delivering the specimen to the laboratory in a timely manner.
We all need to be more aware of the complexities of our different roles by stepping up our communication efforts and being transparent.
What are some of challenges we've faced in blood banking, and how have we improved?
JF—Blood transfusion is the most commonly performed procedure in the United States, and blood is a real scarcity. Our hospital, like many others, must maintain an inventory of blood so it is always available in case of a large-scale trauma.
We’ve put a lot of effort into reducing unnecessary transfusions and improving blood utilization. Right now we are focused on reducing unnecessary type and screen tests in newborns, decreasing blood waste in the operating room, and improving blood-ordering protocols for cardiac surgeries based on the type of procedure.
Our transfusion medical director and manager collaborate with clinical teams to minimize blood transfusions through improved management of patients with anemia and bleeding. They also consult and educate on transfusion protocols.
What have we done to help phlebotomy services run more smoothly?
“We’ve had to learn how to advocate for the lab, solve problems, and collaborate in a system-wide approach, not in a vacuum.”
Jo D Fontenot, ARUP
JG—We’ve moved away from traditional rounding—which involves drawing blood at intervals—to on-demand phlebotomy services. Implementing use of electronic handheld devices made this possible by transmitting and dispatching real-time orders rather than relying on scheduled roundrking diligently behind the scenes
We’ve also implemented bedside labeling that instantly lets the laboratory know the patient’s most current blood orders. This helps avoid unnecessary tests and decreases the risk of mislabeling or lost labels.
How do we develop an engaged workforce?
JF—We’ve invested a lot of effort in this area. To help show appreciation, we require supervisors to spend at least two hours a month expressing gratitude to employees. This might entail writing thank you cards or taking an employee to lunch.
We’re sticklers about making sure our leaders are good leaders who can model good behavior and focus on team building. We assign a mentor to new employees, and their manager follows up at the three-month mark to see how things are going.
All our departments have weekly huddles where the supervisor and/or employees recognize and thank each other for their efforts. These recognitions can show up in their performance reviews. In the huddles, employees can point out lab issues or potential areas of trouble and collaborate in finding a solution. Since we started the huddles, engagement scores have shot up.
JG— Another area that has helped with engagement is our Best in Class initiative, which empowers employees and gives them a sense of ownership. This initiative provides training and tools for the entire staff to improve processes and patient care. It encourages staff to not only identify issues, but also to be a part of finding the solutions. We believe this, too, has prompted the rise in our employee engagement scores.
How have we improved collaboration efforts with the nursing staff?
JF—Nursing staff collects half of the samples sent to the lab, so strengthening the labs’ communication and collaboration with nurses was key for us. With representation from multiple areas, including nursing, the LPI committee has helped address issues impacting patient testing and care. It has proven to be very successful in solving problems from a systems approach and helps medical staff see the bigger picture of what is going on and how they can help solve problems.

For example, the computer system may cancel a duplicate order and send out a “canceled” notification. But the provider assumes the lab has dropped the ball because it is not apparent in the provider’s system that the computer, not the lab, canceled the test. With two different computer systems, issues like this come up. This is one reason why we are moving to Epic’s Beaker system in order to provide more transparency in the medical record.
We also participate in quality meetings with nurses and have formal laboratory liaisons who train nursing personnel on sample processing. If we are getting an increase in specimen issues or complaints from one of our clinics or departments, one of our liaisons will retrain medical staff in that area.
We have to remember that medical staff speaks a different language than lab staff. It’s important to speak their language when communicating concerns to nurses and avoid using too many laboratory-specific terms.
Regarding ARUP’s Huntsman Cancer Hospital labs, what have we learned to do better with regard to caring for patients with cancer?
JF—We are actively involved with the healthcare team in the delivery of care; this includes providing rapid testing, bone marrow support, and on-site and telepathology.
JG—The needs of this patient population are different from our traditional inpatient population. They may be coming in weekly for chemotherapy and their turnaround times (TATs) have to happen a lot faster. In order to improve, we had to reevaluate these patients’ needs and backward engineer to meet those TATs. This led to establishing on-site laboratories for all the Huntsman healthcare system’s infusion centers.
JF—We oversee on-site transfusion at each of the four Huntsman infusion centers. This proximity was key to keeping the coordination tight and the workflow quick. Pharmacists rely on the lab test results to know what chemo dosages patients will need within the hour.
Additionally, we have learned to work closely with nursing and pharmacy staff to ensure we are meeting the needs of patients who are receiving treatment. The area where this has been most challenging is in bone marrow collection, where too often we are not alerted in advance that our bone marrow techs will be needed. This is really about better communication between the care team and the lab, and we are working on it.
JG—We’ve also brought on new testing unique to this patient population; some examples are tumor marker tests and a parathyroid hormone test for intraoperative cases.
When consulting with our clients on site visits, what do they want to know?
JG—They want to know how we’ve tailored our laboratory information system (Cerner PathNet) to meet our needs and what implementation strategies are necessary to do this. We had to find some creative solutions to address common laboratory problems such as how to accommodate add-on testing and tools used for data mining. We share our solutions with our clients in hopes it will help them provide even better patient care.
“Once we showed how integral laboratory services were in the whole hospital’s healthcare system and in patient care and satisfaction, hospital leadership was astonished.”
Jo D Fontenot, ARUP
They are also interested in how to improve lab communications with the hospital and our problem-resolution strategies. For example, they want to learn more about the Except system ARUP developed to allow us to document testing issues without interrupting the workflow.
How have ARUP’s hospital laboratories attempted to resolve communication issues in order to improve efficiencies and avoid errors?
JF—We work with leadership from ARUP and U of U Health to support solutions that resolve problems. We noticed that pharmacy had a medicine safety committee that would report up to the hospital’s safety committee. Yet we didn’t have anything similar, even though labs come in second to pharmacy for being one of the areas where there are the most complaints or nonconformance issues.

Once we pointed this out and showed how integral laboratory services were in the whole hospital’s healthcare system and in patient care and satisfaction, hospital leadership was astonished. As a result, we created the LPI committee I mentioned earlier.
JG—Face-to-face interactions improve communication. We are present in a lot of quality management meetings—in nursing, the intensive care unit, newborn and delivery, and the emergency department, to name a few. We are there to answer questions, find solutions, and help them understand how their actions can impact the lab process.
Lab IT also works with U of U Health’s patient safety reporting system to solve process problems and to improve workflows between the laboratory information system and the hospital’s electronic medical record system.
JF—We’ve been able to jump over a lot of hurdles and find solutions that benefit everyone by focusing on communication, collaboration, and transparency.

















 HOME
HOME