
While COVID-19 has dramatically altered workplaces around the globe, in ARUP’s Infectious Disease (ID) Division, much remains the same. In its 35-year history, this division has tested for the H1N1 virus, Zika virus, and now SARS-CoV-2 with highly trained medical laboratorians using sophisticated instrumentation and following rigorous safety protocols.
Some of the 300 types of infectious disease for which ARUP performs tests are more infectious than others. Specimens being tested for tuberculosis (TB), for example, are handled in a separate room beneath a biosafety hood by laboratorians wearing N95 masks. “TB is by far more lethal and infectious than COVID-19, it’s just not as prevalent,” said Diana Mohl, operations director, Infectious Disease.
Since the start of the COVID-19 pandemic, the ID Division has followed well-established protocols for respiratory specimens. “There has been a decrease in the specimens involving blood, stool, urine, and CSF [cerebrospinal fluid], and a significant increase in specimens … such as respiratory swabs, sputum, nasal, and bronchial washings,” Mohl said.
Preparing for COVID-19: Risk Assessments
In January, ARUP began discussing potential risks associated with COVID-19 testing as part of a proactive effort to protect employees from exposure to the virus.
“Risk assessments are crucial in identifying where you have exposure hazards so you can modify procedures or equipment to mitigate risk,” said Tom Wachter, director of ARUP’s Corporate Safety Department.
With COVID-19, the highest risk areas are those where aerosol generation, spills and splatters, and droplets are possible, he said.
Safety has taken a three-pronged approach to mitigate risk. It has focused on engineering controls (e.g., negative pressure rooms, ventilation systems, biosafety cabinets), procedural controls (e.g., pipetting technique, proper hygiene), and personal protective equipment (PPE).
ARUP has always continuously evaluated and improved safety in its labs. With more than 65 labs, all of which are currently operating, it is business as usual inside the labs. What is new, and not as easy to control, is the risk of COVID-19 exposure outside of the labs and the potential shortages of PPE and other supplies.
Initial sample preparation is done in a class II biosafety cabinet and in a negative air-pressure room in case something spills outside of the biosafety cabinet. A ventilation system is used to create negative pressure to prevent air from flowing out of the room. This air is also 100 percent single-pass fresh air and is completely replaced at least every 10 minutes.
Then new COVID-19 instrumentation automates the transfer of reagents and specimens to plates for molecular testing, so fewer manual manipulations are required of the technician.
All bench tops and contact surfaces are on schedules for disinfection with appropriate Environmental Protection Agency (EPA)-registered disinfectants.
Everyone working with COVID-19 samples wears appropriate PPE for protection, including gloves, lab coats, and N95 masks or powered air-purifying respirators (PAPRs) where necessary. Fit tests for N95 masks are performed to ensure they fit well and function. Lab spill kits have been updated and include impermeable shoe covers.
Safety has also worked closely with suppliers to vet new disinfectants and test PPE to ensure they work well.
To achieve physical distancing in the labs, fewer people are assigned to each shift and individual tasks are spread out within the space available. In areas where workspace configuration prevents physical distancing, laboratorians wear face shields or masks.
Control the Controllable
ARUP has always continuously evaluated and improved safety in its labs. With more than 65 labs, all of which are currently operating, it is business as usual inside the labs. What is new, and not as easy to control, is the risk of COVID-19 exposure outside of the labs and the potential shortages of PPE and other supplies.
To keep employees healthy, ARUP has taken measures that include the following:
- Entry to lab buildings is restricted to essential personnel only.
- Most nonlaboratory employees are working from home.
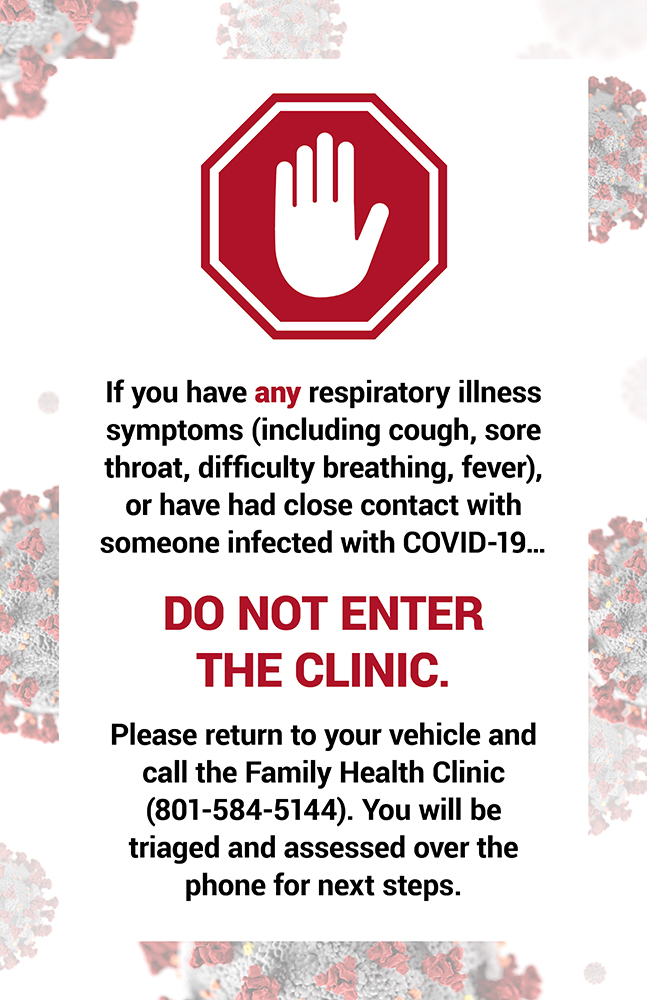
- The on-site Family Health Clinic is assessing symptomatic employees and referring them for COVID-19 testing if necessary. The clinic is also performing contact tracing for anyone exposed to the virus.
- Meetings are being conducted online or by telephone whenever possible.
- To enforce physical distancing requirements, seating in common areas, including the cafeteria, has been reduced or removed.
- Employees are required to complete mandatory training about physical distancing.
“We deal with this type of organism all the time [in the labs],” Wachter said. “It’s the things that we cannot control in this evolving pandemic that make it tricky.”
















