Vascular anomalies are often the result of abnormal development in blood vessels; they may be physically apparent at birth as a blemish or a mass, or show up later in life. About one in 5,000 people experience some kind of vascular anomaly.
When the doctor examined a large reddish rash splashed across the leg of her 16-year-old patient, she suspected it was a type of vascular anomaly (VA). What she didn’t expect is that the genetic test used to classify the malformation would reveal information that could very well save the patient’s father’s life.
Vascular anomalies are often the result of abnormal development in blood vessels: capillaries, veins, arteries, or lymphatics. About one in 5,000 people experiences some kind of vascular anomaly, sometimes as an inherited condition.
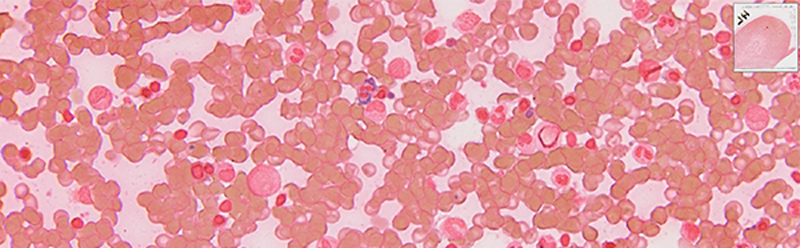
The VA might be physically apparent at birth as a blemish or a mass (infantile hemangiomas) or may appear in later years, as it did for this 16-year old boy, when blood flow increases.
Sometimes unseen, these abnormalities may be buried deep inside the body, only visible via an ultrasound or MRI. They can be fatal, especially those with high blood flow within vital organs such as the lungs or brain. “Most vascular anomalies are isolated, but some can be associated with deeper lesions,” says Alice Frigerio, MD, PhD, a University of Utah Dermatology resident who specializes in VA research.

“There are so many different clinical scenarios that guide workup and treatment,” adds Frigerio. For example, if an infant has more than five hemangiomas on the skin, this should prompt imaging of the liver for possible deeper lesions. If a child was born with a port wine stain on the forehead and/or cheek, it might indicate Sturge-Weber syndrome, which can involve glaucoma or also intracranial lesions that might cause seizures. Hemangiomas on the jaw line may indicate deeper airway issues—present in 50–60 percent of patients—prompting clinicians to look for airway symptoms.
“There are many different types of vascular malformations, potentially affecting any vessel [artery, vein, capillary, lymphatics] developing incorrectly in the fetus" explains Frigerio.
Why Order a Genetic Test?
Most vascular anomalies can be diagnosed and treated based on clinical symptoms without a genetic test. However, there are cases when clinicians may want more information; for example, they may want to determine if the VA is an inherited condition to identify and screen additional at-risk family members, or to gain a deeper understanding of the underlying molecular mechanisms to further tailor treatment.
When doctors suspect a VA, they can order a genetic test (using a blood sample) that utilizes next-generation sequencing (a process used to analyze DNA and its many genetic variants) to investigate the 14 known genes involved in VA. ARUP was the first in the country to develop such a test (Vascular Malformations Panel, Sequencing and Deletion/Duplication), which can identify seven different types of VAs.
“It can help doctors rule out other possible disorders or it can be used to identify the specific type of vascular anomaly,” says molecular genetics expert Pinar Bayrak-Toydemir, MD, PhD, a medical director of ARUP’s Molecular Genetics and Genomics laboratories.
Individual tests on each subtype can be ordered if the doctor already knows what type of VA the patient has but wants a more thorough analysis of the genes involved.
When this VA panel test was performed on the 16-year-old boy with the rash, it identified disease-causing mutations in three genes. One was linked to the skin lesions or capillary malformations (found on the boy’s leg) and was also linked to another vascular malformation in the brain, alerting the clinician to look for symptoms resulting from possible neurological issues.

Molecular genetics scientists Drs. Bayrak-Toydemir and Wooderchak-Donahue (top left and bottom left, respectively) and genetic counselor McDonald are all involved in helping clinicians and their patients identify different types of vascular anomalies through a test that analyzes 14 known genes. ARUP was the first in the country to develop such a test.
As a result of these findings, his parents were tested, and each was found to have two of the three gene mutations (as did his sister). One of these genetic mutations was indicative of colon cancer, prompting the father to get screened. “He had over a hundred polyps that needed to be tested for cancer. It [the VA panel test] most likely saved his life,” says Bayrak-Toydemir. Both the boy’s sister and mother carried two gene mutations that were linked to cancer and vascular anomalies. Such information is important for medical management and family planning.
“Some of the vascular malformation syndromes may cause cancer. There’s not a direct link for everyone; it’s more like a predisposition,” says researcher Whitney Wooderchak-Donahue, PhD. Both she and Bayrak-Toydemir are internationally recognized for their research involving vascular anomalies.
The More We Discover
These two ARUP scientists are working on a test that screens lesion tissue and blood from patients. “This will give us a more comprehensive view, and we’re more likely to identify additional positive cases,” says Wooderchak-Donahue. She explains that if the biomarkers are in the blood cells, the VA is more likely to be passed on to future generations. If it is just in the tissue, it is limited to that individual.
In a recent case published last June in the American Journal of Medical Genetics, Wooderchak-Donahue and Bayrak-Toydemir showed that a patient’s capillary malformation lesion was caused by a second somatic hit in the same RASA1 gene, which caused complete loss of function of both copies of the gene and the formation of the vascular lesion. Currently, they are collaborating with Stanford scientists on an additional study to further investigate this aspect.
“There is a lot of effort worldwide in the vascular anomaly community to understand the molecular mechanisms; this is laying the groundwork for new therapies,” says Frigerio. This was evident for lymphatic malformations, for which scientists were able to identify molecular mechanisms that prompt the malformation to continue growing. Scientists were able to develop a drug to turn off this growth signal.
“The more we study, the more we discover, the more we understand, and the more we can develop new treatments,” adds Frigerio, who came from Harvard to join the ARUP team because of the dynamic research environment happening in this area.
Peta Owens-Liston, ARUP Science Communications Writer